by Sanjay Pithadia, System Engineer, Medical Sector, System Engineering, and Marketing atTexas Instruments
Health care continues to evolve toward self-treatment and away from in-person appointments. In addition to helping reduce physical contact, new technologies have given the general population unprecedented access to health care tools for self-monitoring and remote treatments. Whether it’s providing mobility to an aging population, helping with infectious disease containment, reducing emergency response times, or delivering health care to rural areas, telehealth has become invaluable in times like these.
In this article, I’ll describe newer technological developments that have greatly affected the telehealth and telemedicine industry, along with associated design challenges for both hospitals and homes. These challenges include how to sense vital signs, minimize power consumption, increase accuracy and reliability, improve connectivity, and squeeze features into size-constrained applications.
Addressing design challenges in biosensing applications
There is typically a high level of complexity in designs associated with biosensing and wearable medical devices. Figure 1 shows how it’s possible to monitor multiple patients at different locations wirelessly, with their vital signs shown on a monitor at a hospital’s nurses station. Because the use case can vary from patient to patient, the design complexity also increases in power consumption, size, and connectivity.

Analog front-end (AFE) devices – which assist with interfacing digital electronics to the noise, time- and light-sensitive sensors used in medical applications – have significantly impacted telehealth end equipment such as pulse oximeters and heart-rate monitors. AFE devices help manage the typical challenges associated with medical applications, including reliability in patient-monitoring systems, power consumption for wearable devices, and flexibility for nonstandard peripherals.
Biosensing AFEs support heart-rate monitoring and variability, a saturation of peripheral capillary oxygen (SpO2), hearing aids, and optical blood-pressure measurements, along with many other biosensing functionalities. AFEs such as the AFE4400 come fully integrated with on-chip optics and diagnostics for sensing and LED fault detection, improving pulse-oximetry systems’ reliability. Highly configurable timing controllers for nonstandard connections and ultra-low-power features that enable low quiescent current during normal and standby operation make AFEs a good fit for compact, battery-powered wearable electronics and optical-based measurements and monitoring.
In addition to pulse oximetry, wearable temperature patches are an emerging trend in patient temperature-monitoring applications. Given that body temperature can help reveal at-risk patients’ medical status, these patches have become increasingly popular for those who require continuous remote monitoring and are available at fairly affordable price points. Temperature measurements conducted for medical diagnostics must meet the American Society for Testing and Materials maximum error values, and meeting these values requires several design considerations. For example, one way to reduce the error value is to make good thermal contact while isolating other ambient heat sources.
Figure 2 shows the Multiparameter Front-End Reference Design for Vital Signs Patient Monitor, a battery-powered multiparameter patient-monitoring design for measuring vital signs such as the heart’s electrical activity SpO2, or respiration. This system uses multiple AFEs and temperature sensors to accurately measure pulse characteristics, electrical activity, and skin temperature (±0.1oC) while providing connections to pace-detection modules for pacemaker detection applications. Although it’s common for biosensing applications to require configurable gains and data rates due to the nature of electrodes and fluctuating optical signals, using a highly programmable analog-to-digital helps manage the biopotentials.

Power optimization
Because they’re designed to measure and monitor continuously, portable, and wearable patient monitors are typically battery-powered, making battery life a differentiator between products. Battery-powered systems require careful partitioning, smart use of little space, and efficient power consumption. Patients and physicians want more efficient features in smaller packages and longer times between recharging – that’s a tall order for a battery.
Designers can use low-power microcontrollers (MCUs) and analog ICs, but they won’t leverage most of the latest technologies in a design unless they optimize power management. The power architecture must be as efficient as possible and have extended battery run times.
For battery-powered designs incorporating an MCU, leveraging power-saving functions such as sleep, hibernate, and shutdown can help greatly extend battery life. Wakeup times and standby power consumption also play vital roles in wireless connectivity.
In addition to digital power-saving options, designers must also consider analog power-management components such as regulators or DC/DC converters to maximize efficiency, incorporating load switches to disable peripherals when not using and selecting the battery type and optimizing its charge profile.
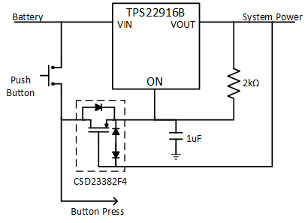
Ship mode uses several components to prolong battery life during the shipment and shelf life of battery-powered electronics such as wearables. For example, the TPS22916 load switch can act as a noninvasive circuit separate from the main electronics, minimizing leakage and disconnecting the battery from the system through a general-purpose input/output signal dedicated to an MCU pin or through abutton. Figure 3 demonstrates the simplicity of this circuit.
In addition to power management during shipping and storage, battery-life monitoring, reporting, and prediction has improved greatly with the use of fuel-gauge ICs that are cost-effective and offer ultra-low power-consumption features.
Connectivity technology for remote monitoring systems
In addition to power, connectivity is another critical aspect of patient-monitoring systems and remote health care devices. Patient monitors requiring crisp and clean displays with high-resolution visualization and readouts may require high-speed or dual-core processing.
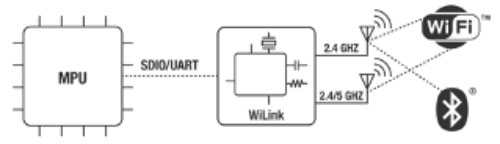
While faster processing is useful for displays, there are some major challenges around wireless connectivity, such as latency and high-data-rate requirements for real-time vital sign display. Wireless modules such as TI’s WiLink 8 device family contain dual-band Wi-Fi®, Bluetooth®, or a combination of both (Figure 4); these modules are meant for applications with throughput up to 100 Mbps and complement the Sitara processor. They provide enterprise-level Wi-Fi security, Wi-Fi Protected Access 3, and Federal Information Processing Standards 140-2 certification from the U.S. government.
Another challenge with designing for wireless connectivity, specifically with wearable devices, is high-power use associated with radio transmission and the management of bulky radio modules in compact applications.
Data security
Wireless medical sensor patches and patient monitors need best-in-class security. Patient data is proprietary information, and data theft is a serious threat.
There are already several security measures designed to protect intellectual property (IP) and data sent between patients and physicians. These measures should protect against attacks and secure data transmissions, not only while processing and converting to vital-sign parameters for display but also during transfer. This is called over-the-air security.
While AFE biosensing devices with optimized form factors, multimodal sensing, and power consumption have given design engineers highly useful tools and components for developing telehealth applications, combination MCU/radio devices, and multicore processors have also enabled remote applications in which high-throughput, continuous data streaming is critical for patient visualization and readouts like continuous vital sign displays at nurse stations.
Conclusion
As biomedical designers resolve challenges and deliver better wireless patient monitors and patches to market at more affordable prices – and in smaller sizes, but with connectivity – the medical world will evolve rapidly. From hospitals in developed countries to telemedicine centers in developing countries to the triage of injured soldiers in the field, wearables will change the health care landscape and help provide better care.